Coronary Artery Disease (CAD)
Learn about CAD through its symptoms, treatments, preventative measures, anatomy and physiology, biological mechanisms behind CAD, and more.
HEART DISEASE
Avya Patel, Ayush Patel
3/17/20258 min read
Coronary Artery Disease: CAD
What is CAD?
CAD is the most common form of heart disease, and the leading cause of mortality in the US. Around 1 in 4 deaths are as a cause or associated with CAD, totaling to around 610,000 deaths in the US alone per year, with 17.9 million deaths worldwide per year.
Coronary Artery Disease (CAD) is a condition where the coronary arteries become clogged, narrowed, or blocked due to a plaque buildup. Plaque is made up of fatty deposits, cholesterol, and other substances that accumulate in the artery walls over time, leading to a process called atherosclerosis, atherosclerosis can occur due to vascular calcification of heart walls, valves and blood vessels. As the arteries become narrowed, blood flow to the heart muscle is reduced, this process is called ischemia, which can lead to chest pain (angina), myocardial ischemia (lowered blood supply to heart muscle), shortness of breath, and, in severe cases, heart attacks.
The general risk factors of CAD include high blood pressure, high cholesterol, smoking, diabetes, a sedentary lifestyle, and a family history of heart disease. Preventive measures involve managing these risk factors, eating a heart-healthy diet, exercising, and taking medications as prescribed such as calcium blockers, lipid blockers, beta blockers, and more. Surgical interventions for CAD include angioplasty or coronary artery bypass grafting (CABG) and others.
In generality, the causes of CAD can be differentiated into atherosclerosis, vascular inflammation, and plaque instability.
The Anatomy and Physiology of Basic Coronary Circulation:
Before getting into CAD in general, it is essential to understand how coronary circulation works and the mechanisms done to promote coronary circulation.
Anatomy:
With CAD, major coronary arteries are first to develop atherosclerosis and plaques, the most common cases of CAD lie in the Left Coronary Artery (LCA), recall that the LCA divides into the Left Anterior Descending (LAD) and Left Circumflex Artery (LCX) and the Right Coronary Artery (RCA).
Physiology:
The Coronary Arteries normally flow during diastole (period when the heart muscle is relaxed and the chambers fill with blood) because during systole (contraction of the heart muscle when the chambers expel blood), the coronary arteries are compressed during contraction.
The vasodilation and vasoconstriction behind coronary arteries is regulated by the endothelium; the endothelium releases nitric oxide (NO) for vasodilation, and endothelin-1 for vasoconstriction. In coronary circulation, the blood demand for the Myocardial muscle is influenced by heart rate, contractility, and wall tension.
Taking this into consideration, any impairment of coronary circulation regarding the physiology can lead to an ischemia and in severe cases, myocardial infarction. In the case of CAD, CAD impacts circulation on a biological level and will be discussed below.
Biological mechanisms of CAD:
Pathophysiology:
In terms of biological mechanisms that contribute to CAD, both genetics and lifestyle play a major role in dictating the probability of CAD.
When examining root causes of CAD at the biological level, it is essential to look at the biological mechanisms attributed to atherosclerosis. The plaque in atherosclerosis is consisted of:
Lipid buildup which stems from lipid deposition: Low-density lipoprotein (LDL) cholesterol infiltrating the endothelium of a coronary artery.
Endothelial dysfunction: Dysfunction of the endothelium can happen for a variety of reasons, the major ones being hypertension, smoking, or high blood sugar which disrupt normal nitric oxide production from the endothelium, reducing vasodilation.
Inflammation: Macrophages engulf oxidized LDL, forming foam cells, which contribute to fatty streaks.
Fibrous cap formation: Smooth muscle cells migrate and form a collagen-rich cap over the plaque, the fibrous cap forms because smooth muscle cells migrate in response to pro-inflammatory signals.
Plaque rupture and thrombosis: If the fibrous cap ruptures, platelets aggregate, leading to a clot that can occlude the artery and cause myocardial infarction (heart attack).
Cellular and Molecular Biology of CAD pathophysiology:
Knowing that the key molecular events include lipid accumulation, oxidative stress, chronic inflammation, and endothelial dysfunction.
The complex interplay of cellular and molecular mechanisms which contribute to atherosclerosis, vascular inflammation, and plaque instability are listed below:
Endothelial Dysfunction:
Endothelial dysfunction, and later CAD stems from risk factors such as hypertension, hyperlipidemia, smoking, and diabetes lead to endothelial dysfunction, reducing nitric oxide (NO) bioavailability. In addition, oxidative stress increases due to excessive reactive oxygen species (ROS), impairing vasodilation and promoting inflammation.
· Lipoprotein Deposition and Modification:
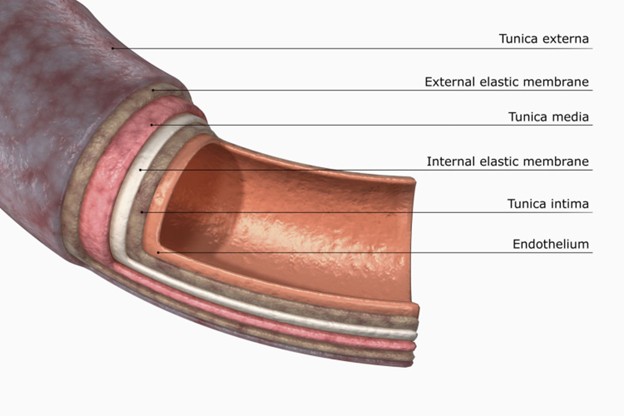
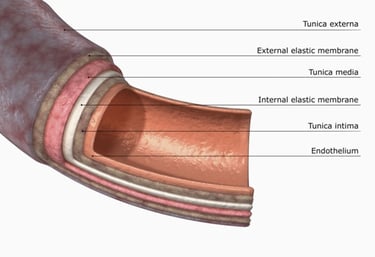
Low-density lipoprotein (LDL) particles infiltrate the intimal layer of the artery.
LDL undergoes oxidation (oxLDL) due to ROS, making it more immunogenic and pro-inflammatory.
Macrophages engulf oxLDL through scavenger receptors, forming foam cells, a hallmark of atherosclerosis, this triggers formation of foam cells triggers a cascade of inflammatory responses, further enhancing atherosclerosis, this section is discussed in monocyte differentiation into macrophages.
With the case of Endothelial Dysfunction where the release of NO is inhibited, such formation of oxidative LDLs and further inflammation enhance the cascade of atherosclerosis and CAD.
Inflammatory Response and Foam Cell Formation:
Coming from oxLDL production and migration of macrophages arises inflammatory responses as a result of foam cell formation.
The immune system recognizes oxLDL as foreign, triggering an inflammatory cascade.
The immune system recognizes oxLDL as foreign, triggering an inflammatory cascade.
Monocytes are recruited to the endothelium via adhesion molecules (e.g., VCAM-1, ICAM-1).
Monocytes differentiate into macrophages, which engulf oxLDL, forming lipid-laden foam cells.
Foam cells secrete pro-inflammatory cytokines such as TNF-α, IL-1β, IL-6, and chemokines like MCP-1, amplifying inflammation.
Smooth Muscle Cell (SMC) Migration and Proliferation:
Vascular smooth muscle cells (VSMCs) in the media migrate into the intima (diagram above) in response to growth factors.
VSMCs switch from a contractile phenotype to a synthetic phenotype, promoting extracellular matrix (ECM) deposition.
The switch of such phenotype is associated with CKD patients in which atherosclerotic plaques are exaggerated due to the high levels of FGF-23 and its conjugate receptors (this phenomenon will be elaborated in a future research article).
This process leads to the formation of a fibrous cap, which stabilizes the plaque, however, this fibrous cap is prone to rupture, causing a wide variety of complications because of factors above.
Thrombosis of the Fibrous Cap:
After the foam cells (when macrophages engulf oxLDL) go under apoptosis, the fibrous cap around the plaque starts to degrade.
The plaque ruptures causing platelets to aggregate on it because of glycoprotein IIb/IIIa receptors, forming a thrombus/blood clot.
This blood clot causes myocardial ischemia, ACS (acute coronary system), or myocardial infarction (heart attack).
Symptoms of CAD:
Since CAD can evolve over a span of multiple years, however, a plaque rupture mentioned above, leading to a thrombosis can occur rapidly, the onset of pain can lead to a myocardial infarction if not given proper attention or treatment within several minutes.
Over a span of multiple years, the symptoms may include:
Fatigue, shortness of breath, and other symptoms may also come on gradually as the heart becomes less efficient at pumping blood.
Chest pain (angina) that occurs intermittently, often triggered by physical activity or stress.
Sudden onset symptoms as a result of a thrombosis or a plaque rupture can include:
Severe chest pain
Sudden shortness of breath
Dizziness or fainting
Pain in other areas of the body: Pain may radiate to the shoulders, arms (usually the left arm), back, neck, jaw, or even the abdomen); these pains are normally associated with a rapid onset myocardial infarction.
Risk Factors:
Controllable risk factors:
High blood pressure (Hypertension): Persistent high blood pressure puts strain on the heart and arteries, increasing the risk of CAD, hypertension often arises from genetics or an unhealthy died, however can be managed by both medication and dietary changes.
High cholesterol levels: Elevated levels of low-density lipoprotein (LDL) cholesterol and triglycerides, along with low levels of high-density lipoprotein (HDL) cholesterol, contribute to plaque buildup in the arteries.
Smoking: Smoking damages the lining of the arteries, raises blood pressure, and decreases oxygen supply to the heart, significantly increasing the risk of CAD.
Physical inactivity: A lack of exercise contributes to weight gain, high blood pressure, high cholesterol, and poor cardiovascular health.
Unhealthy diet: Diets high in saturated fats, trans fats, cholesterol (especially LDL), salt, and sugar can contribute to high cholesterol, high blood pressure, and obesity, all of which are CAD risk factors.
Excessive alcohol consumption: Drinking alcohol in large quantities can raise blood pressure and contribute to heart disease.
Stress: Chronic stress, along with unhealthy coping mechanisms like smoking, overeating, or drinking alcohol, can contribute to CAD.
Uncontrollable risk factors:
Age: The risk of CAD increases as people age. Men typically develop CAD earlier than women, but the risk for women rises after menopause.
Gender: Men generally have a higher risk of CAD (around 10-17%) at a younger age, but women’s risk increases and may surpass men’s risk post-menopause.
Family history of heart disease: A family history of heart disease or early heart attacks can increase an individual's risk.
Genetics: Some people may inherit genes that increase their risk of developing CAD, such as those that influence cholesterol levels, blood pressure, or other cardiovascular factors.
Ethnicity: Certain ethnic groups (e.g., African Americans, Hispanics, and South Asians) may have a higher risk of developing CAD due to genetic and lifestyle factors.
It is important to note that diseases such as obesity and diabetes that influence CAD can be both inherited through genetics but can also be developed due to an unhealthy lifestyle and diet.
Other risk factors:
Sleep apnea: Untreated sleep apnea can increase the risk of hypertension, atrial fibrillation, and CAD.
Inflammatory conditions: Conditions like rheumatoid arthritis and lupus may increase CAD risk due to chronic inflammation.
CKD as an autoimmune condition increases rates of vascular and coronary calcification due to a cascade of smooth muscle cell differentiation into osteoblastic differentiation, a similar method as SMC proliferation and migration above.
Complications:
Several complications can arise from prolonged, undetected, and untreated CAD with the most known and notable being an ischemia, myocardial infarction, strokes, arrythmias…
From the following complications below, heart failure is a large cause for concern where the heart is unable to pump blood effectively to meet the body's needs. This happens when the heart muscle is damaged over time due to inadequate blood supply.
Myocardial infarction: In a sudden or prolonged instance where blood flow to the heart muscle is cut off due to lipid deposits or blood clots, the contractile heart muscle cells die rapidly, and in severe cases, causes a portion of the heart muscle to die.
Angina: Angina/ chest pain can happen over the course of CAD or rapidly, in the case of gradual chest pain, exertion or stress can create a feeling of pressure or sharp pain. Over time, an angina can worsen to become an unstable angina which is more frequent, severe, and can occur at rest, increasing the risk of heart attack.
Arrythmias: Irregular heart rhythms can take form as atrial fibrillation or ventricular fibrillation, leading to sudden cardiac death (more specifics of such rhythms will be discussed later).
Stroke: Accompanied with CAD can come plaque buildups in the brain’s arteries, like thrombosis in coronary arteries, such clots can form in the brain, leading to a stroke.
Aneurysm: An aneurysm occurs when a blood vessel wall weakens and bulges. In CAD, this can happen in the aorta which can lead to a risk of rupture such as an aortic dissection, which can be fatal.
Peripheral Artery Disease (PAD): The arteries supplying blood to the limbs and other parts of the body (through the peripheral circulatory system) become narrow with a major reason being hypertension. PAD can lead to pain, infection, and even limb amputation in severe cases.
Chronic Kidney Disease (CKD): CKD and CAD are often interconnected through various molecular biological mechanisms. Reduced blood flow to the kidneys can lead to dialysis or even kidney transplantation.
Treatment + Preventative Options:
For CAD, treatment options often must be considered alongside the risk factors for CAD. Lifestyle changes, medications, and procedures (both interventional and surgical options) are common interventions to treat or control CAD.
In terms of lifestyle changes, the most prominent and foundations of CAD treatment are healthy diet which contain a heart-healthy diet (low in saturated fats, trans fats, sodium, and cholesterol) can help lower cholesterol and blood pressure. In addition, exercise and weight management are crucial to improving heart function and reduce the risk of developing secondary diseases.
With medications come a broad-spectrum including anticoagulants like aspirin to lower the risk of blood clots, statins to lower the levels of LDL, Beta-blockers and ACE inhibitors or ARBs: to lower blood pressure and strain on the heart. Furthermore, calcium channel blockers help increase vasodilation, Nitroglycerin (NTG) relieve anginas, and diuretics to reduce fluid buildup in the body.