Basics of the Heart Anatomy: The Major Heart Structures
This article will discuss the rest of the major heart structures including major blood vessels of the circulatory system, the heart walls, the electrical conduction system, and specifics about the heart chambers and valves. The article will include a lot of medical terminology.
ANATOMY AND PHYSIOLOGY
Avya Patel
2/25/202511 min read
The Major Heart Structures
In this article, we will explore the major heart structures and how they all work together. These structures will be recurrent in other articles to help understand the role of these structures and what happens if they do not work as they are supposed to.
The following topics will be covered below:
The heart walls
Major blood vessels of the circulatory system, coronary arteries, and veins
Basics of the heart’s electrical conduction system
Important note: The aorta, pulmonary arteries + veins, vena cava, the heart valves, and the heart chambers were discussed briefly in CardioSphere’s article, Basic Heart Anatomy and Physiology: Introduction to Heart Chambers.
The walls of the heart:
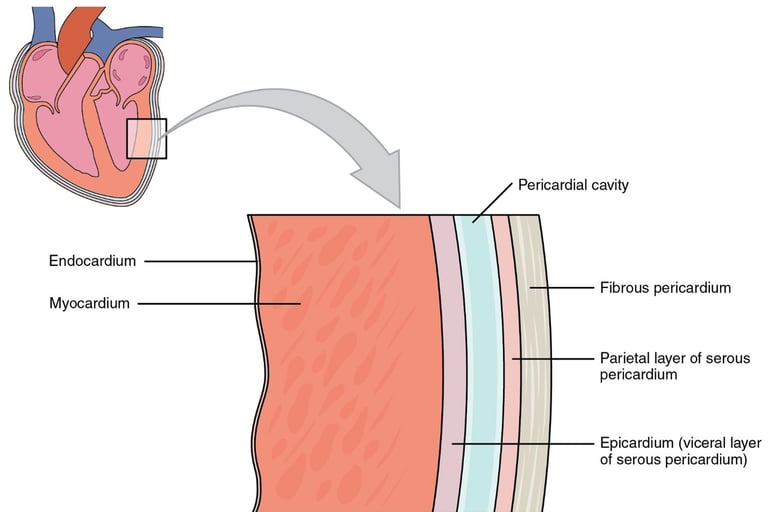
Starting from the inside to outside layers of the heart:
Endocardium
Myocardium
Pericardium
Serous Pericardium
Visceral Layer/ Epicardium
Pericardial Cavity
Parietal Later
Fibrous Pericardium
Endocardium:
The endocardium is the innermost layer of the heart and covers its inner surfaces, including the heart valves and chambers. The endocardium contains an endothelial layer made up of simple squamous epithelial cells (cells that make up your blood vessels). Additionally, the endocardium's endothelial layer is responsible for exchanging materials between the heart and blood vessels. As we get closer to the myocardium, the endothelium (the innermost layer of the epicardium) starts connecting to a form of connective tissue called areolar tissue.
The main functions of the endocardium are:
Maintaining constant contraction of the atrium and ventricles/maintaining constant blood flow out of the heart.
Hosting the SA and AV nodes: They are specialized cardiac tissue (groups of pacemaker cells) responsible for maintaining heart contraction by generating and regulating the heart's electrical impulses.
When in exercise, the myocardium can adapt to changes in stimuli through the help of the pacemaker cells (SA and AV node) and cardiomyocytes by increasing the size of the muscle and increasing pumping efficiency.
Myocardium:
The myocardium is the largest layer of the heart since it contains cardiomyocytes (cardiac muscle cells) and is the layer of the heart responsible for atrial and ventricular contraction, in turn, making the heartbeat. This muscular layer contains the SA and AV node (a major part of the heart’s electrical and conductive system), 2-4 billion cardiac muscle cells (cardiomyocytes), an adequate supply of blood vessels, and many nerves. The myocardium wraps around the atrium in a figure-8 pattern.
The myocardium can be divided into 3 further parts:
Superficial Layer: Outer muscle fibers that wrap around both ventricles.
Middle Layer (in ventricles only): Muscle fibers arranged in a circular pattern (most prominent in the left ventricle since the left ventricle is the largest).
Deep Layer: Inner muscle fibers faced longitudinally/ length-wise, crucial for ventricular contraction.
Epicardium and Pericardium:
The epicardium and pericardium are both connected directly. The pericardium is divided into the fibrous pericardium and the serous pericardium, the serous pericardium can again be divided into two sections, the parietal layer of the serous pericardium and the visceral layer of the serous pericardium (the epicardium), because of this, the epicardium is technically part of the pericardium as it is the visceral layer of the serous pericardium.
Serous pericardium:
Getting into the specifics of each complex pericardial layer, the visceral layer of the serous pericardium (epicardium) is the innermost part of the pericardium; it also connects to the myocardium. Recall that this sub-layer is part of the serous division of the pericardium. This visceral layer also contains a thin lining of cells called the mesothelium and a type of connective tissue called areolar connective tissue. The next innermost layer of the pericardium is the parietal layer. This layer contains both a mesothelium and areolar connective tissue (like the visceral layer), but it also contains a fibrous layer for added protection. In between the visceral layer (epicardium) and the parietal layer lies a cavity called the pericardial cavity.
The main functions of the visceral layer of the serous pericardium are:
Protection and lubrication by shielding the endocardium and myocardium from friction, and support during contraction.
Structural support by providing blood and connective tissue.
A barrier against infection.
The main functions of the parietal layer of the serous pericardium are:
The parietal layer shares many of the same functions as the visceral layer but is more specialized in protection and mechanical stability as it is connected to the fibrous pericardium (a tough outer shell of the heart).
(Martini, F., Nath, J., & Bartholomew, E. F., 2018). Fundamentals of anatomy & physiology (11th ed.). Pearson Education, Inc.)
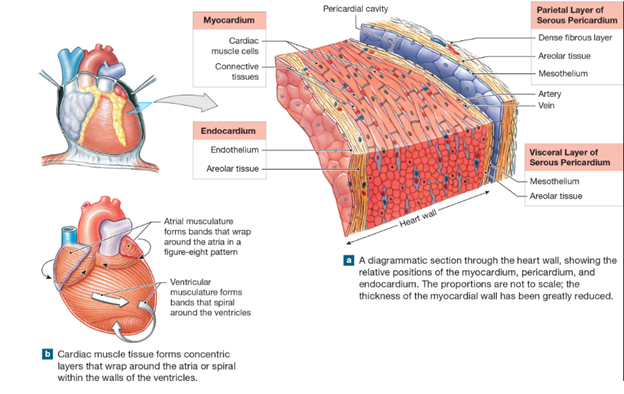
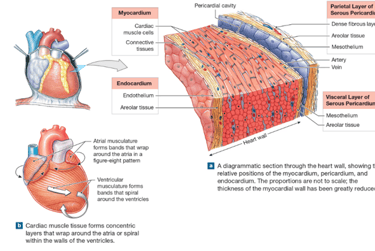
Fibrous pericardium:
The fibrous pericardium does not have further divisions like the serous pericardium, furthermore, it is the last layer connected to the heart and therefore provides the most protection with the use of dense irregular connective tissue (interwoven fibers to increase protection and ensure no breakage during strong contractions). This fibrous layer is made up of collagen fibers to limit excess expansion of the heart and to ensure durability, elastic fibers to allow for some elasticity and contraction of the heart, and finally, cells called fibroblasts that produce more tissues and fibers in case of injury or damage.
The main functions of the parietal layer of the serous pericardium are:
Protection from surroundings.
Anchor the heart into a firm position between the 1st and 5th intercostal space.
The major circulatory system vessels:
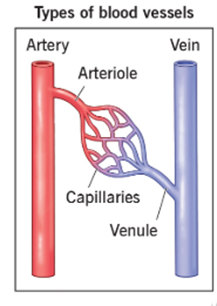
The circulatory system can be broken up into;
Arteries: Carry oxygenated blood to the heart; the only arteries in the body that do not carry oxygenated blood are the pulmonary arteries.
Arterioles: Smaller branches of arteries that branch into capillaries.
Capillaries: Small vessels that help exchange oxygen, waste, and nutrients between blood and tissues.
Remnants can be in the form of CO2, lymph, urea (waste products)… can be taken out by the lymphatic system, to the liver, kidneys, or lungs.
Venules: Since capillaries carry both oxygenated and deoxygenated blood to regulate mineral exchange, venules are used to collect deoxygenated blood to the veins.
Veins: Carry deoxygenated blood to the heart; the only veins in the body that do not carry deoxygenated blood are the pulmonary veins.
(Cleveland Clinic. “Blood Vessels.” Cleveland Clinic, 9 July 2021, my.clevelandclinic.org/health/body/21640-blood-vessels.)
The above diagram from Cleveland Clinic shows how all the classifications of the blood vessels relate to one another. Imagine the capillaries (the small vessel branch toward the center) providing blood to tissues or muscles, deoxygenated blood and waste used up by the muscles enters the capillaries and will eventually end up in the venulesà veins to be transported to the lungs, kidneys, lymphatic system, or liver for waste removal. The role of arteriesà arterioles is then broken down to small capillaries to provide blood and nutrients to muscles.
The major vessels of the body:
The above diagram from Cleveland Clinic shows how all the classifications of the blood vessels relate to one another. Imagine the capillaries (the small vessel branch toward the center) providing blood to tissues or muscles, deoxygenated blood and waste used up by the muscles enters the capillaries and will eventually end up in the venulesà veins to be transported to the lungs, kidneys, lymphatic system, or liver for waste removal. The role of arteriesà arterioles is then broken down to small capillaries to provide blood and nutrients to muscles.
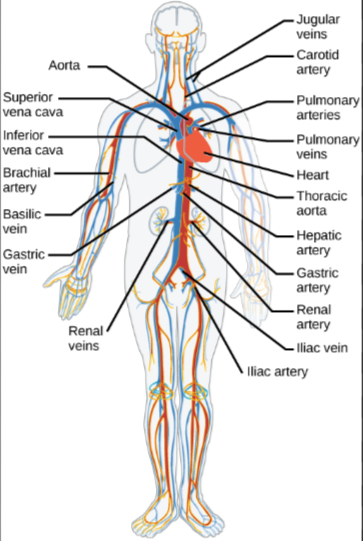
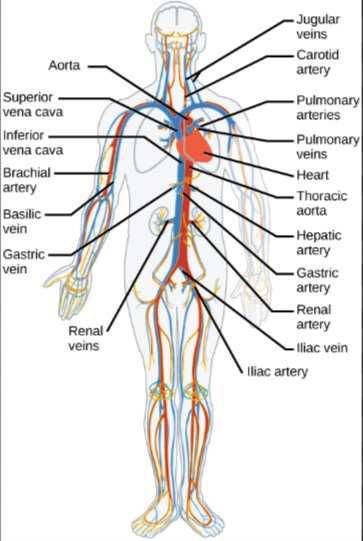
The Peripheral Vascular System (PVS):
The PVS is tasked with supplying and collecting/ draining blood from all body parts, excluding the heart.
The Major Veins of the PVS:
Specifics about the Inferior Vena Cava (IVC):
The inferior vena cava collects deoxygenated blood from venules of the lower extremities, such as the lower abdomen and lower limbs. It is also derived from the iliac veins, which are in the L3-L5 (lumbar divisions of the spine). It travels upward from the abdomen, passing the liver as it makes its way up and continues to run up along the right abdomen cavity and right vertebral column.
The inferior vena cava returns deoxygenated blood from the lower body, including the legs, abdomen, and pelvic region, to the right atrium. The inferior vena cava works along with the superior vena cava (SVC) to continue circulating deoxygenated blood from the body to the right atrium.
Attributing veins connecting/ draining to the IVC:
Common iliac veins (drains pelvis & lower limbs)
Lumbar veins (drains posterior abdominal wall)
Hepatic veins (drains liver)
Inferior phrenic veins (drains diaphragm)
Gonadal veins (right gonadal drains directly, left drains into left renal vein first)
The right gonadal drains directly into the IVC since it is located along the right side of the body.
Renal veins (drains kidneys)
Collects the left gonadal vein before draining into the IVC.
Specifics about the Superior Vena Cava (SVC):
The superior vena cava collects deoxygenated blood from venules of the upper extremities, such as the upper limbs and head. It starts from the 1st costal cartilage (helps make the thorax and serves to prolong the ribs forward during breathing and heart contraction) and enters the right atrium at the 3rd costal cartilage.
The SVC runs vertically down after collecting blood from the head, neck, upper limbs, and thorax, back to the heart's right atrium. It lies to the right of the aortic arch and in front of the trachea and right pulmonary artery.
Attributing veins connecting/ draining to the SVC:
Right and left brachiocephalic veins – Carry blood from the head, neck, and upper limbs.
These two are the main veins that, when merged, form the SVC.
Azygos vein – Drains blood from the thoracic wall and posterior intercostal veins into the SVC just before it enters the pericardium.
Small veins from the pericardium and mediastinum may also drain directly into the SVC.
Specifics about the Jugular Veins:
The jugular vein drains blood from the head, face, and brain to the right atrium. The jugular veins go hand-in-hand with the superior vena cava since all 3 of the jugular veins drain into the SVC.
The 3 jugular veins are:
Internal Jugular Vein (IJV): The IJV’s role is to collect blood from the brain, skull, and neck, which is why it has Major Venous Drainage. This vein later joins the 2 brachiocephalic veins and is discharged into the right atrium
External Jugular Vein (EJV): The EJV is to collect blood from areas beneath the skin from the scalp and face, which is why it has Superficial Drainage. This vein travels close to the skin before merging at the subclavian vein (the subclavian vein joins the brachiocephalic vein complex)
Anterior Jugular Vein (AJV): The AJV’s role is to collect blood from the front surfaces of the neck. Like the EJV, the AJV runs close to the skin and collects minimal blood. The AJV, since it collects minimal blood, collects into the EJV.
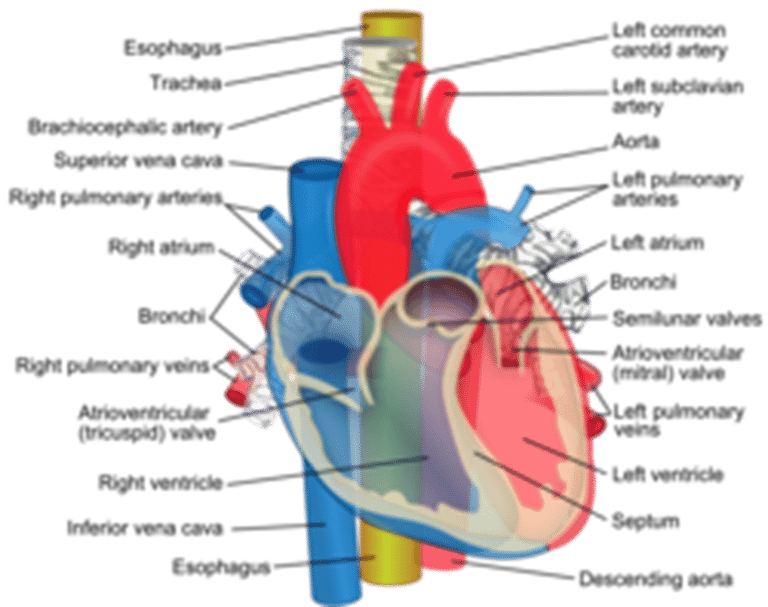
Specifics about the Pulmonary Veins:
The pulmonary veins are a set of 4 veins that return oxygenated blood from the lungs to the left atrium. These veins are unique since they are the only veins in the body that contain oxygenated blood.
4 pulmonary veins (two from each lung, each vein takes blood from different lobes of the lung)
Right superior pulmonary vein – Drains the right upper and middle lobes
Right inferior pulmonary vein – Drains the right lower lobe
Left superior pulmonary vein – Drains the left upper lobe
Left inferior pulmonary vein – Drains the left lower lobe
Specifics about the Aorta:
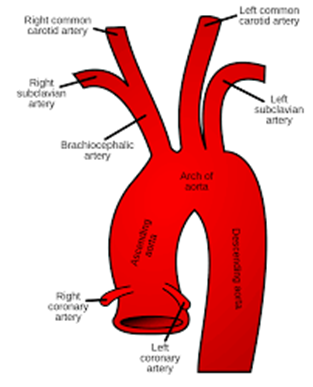
The aorta is the largest artery in the body; it is responsible for giving blood to the body, including the heart. The aorta emerges from the aortic valve from the left ventricle.
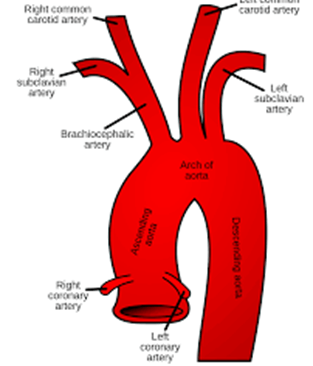
The aortic arch branches into several sub-arteries: the right coronary artery, the left coronary artery, the brachiocephalic artery which branches into the right common carotid artery (mentioned below) and the right subclavian artery, additionally, the aortic arch gives rise to the left common carotid artery (mentioned below) and the left subclavian artery.
Parts of the Aorta:
The Ascending Aorta Begins at the aortic valve from the left ventricle and travels upwards and slightly to the right. The ascending aorta is responsible for branching to the two coronary arteries, which supply blood to the heart: the left and right coronary arteries.
The Aortic Arch: Connecting to the ascending aorta, the aortic arch divides into the Brachiocephalic artery (trunk). → Gives rise to:
Right subclavian artery (supplies the right arm).
Right common carotid artery (supplies the right side of the head and brain).
The left common carotid artery (mentioned below), and the left subclavian artery (supplies blood to the left arm).
The Descending Aorta: The descending aorta must provide blood to the rest of the body not mentioned above. The descending aorta is broken into several sub-aortas (below), eventually leading to major arteries of the peripheral vascular system (PVS)
The Descending Thoracic Aorta: Arteries that rise from this provide blood to the rib cages, esophagus, and lungs.
The Abdominal Aorta: Arteries that rise from this provide blood to the stomach, liver, spleen, kidneys, colon, pancreas, testes, ovaries, and parts of the abdominal wall and muscle.
Finally, the descending aorta branches into the common iliac arteries, which supply blood to the legs and pelvis.
Specifics about the Carotid Arteries:
The carotid arteries, opposite the jugular veins, supply blood to the head and neck. Each side of the neck has a carotid artery, and since the carotid arteries are large, the pulse is often checked here.
The 3 carotid arteries are:
Internal Carotid Artery (ICA) – Major supply of blood to the brain.
External Carotid Artery (ECA) – Supplies blood to the face, scalp, and superficial structures.
Common Carotid Artery (CCA) – Primary Artery
Divided into the right common carotid artery and left carotid artery. The right common carotid artery comes from the brachiocephalic trunk (one of the three main arteries that come from the aortic arch). The left common carotid artery comes directly from the aortic arch.
Specifics about the Pulmonary arteries:
After the opening of the pulmonary valve, the pulmonary arteries transport deoxygenated blood from the right ventricle to the lungs. These arteries are unique because they are the only arteries in the body that contain deoxygenated blood.
3 pulmonary arteries
Main Pulmonary Artery (Pulmonary Trunk)- Arises from the pulmonary valve from the right ventricle
Right Pulmonary Artery (RPA)- Longer and larger than left pulmonary artery
Left Pulmonary Artery (LPA)
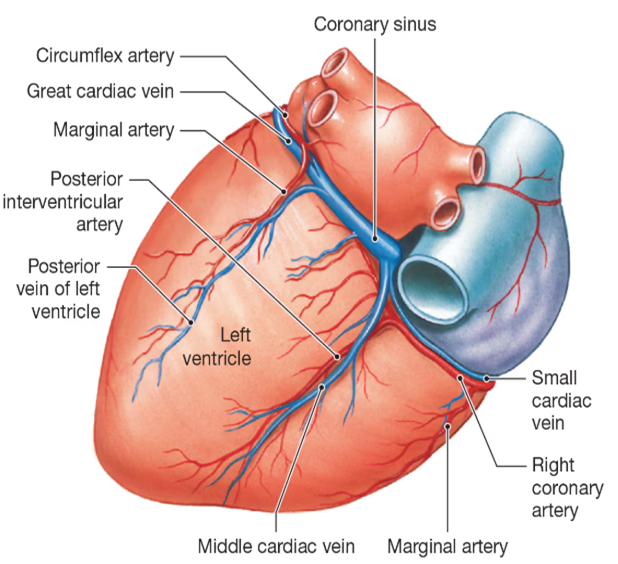
The Cardiovascular/ Coronary System
The cardiovascular/ coronary system is a collection of blood vessels (coronary vessels) that are tasked to drain and provide blood to the heart.
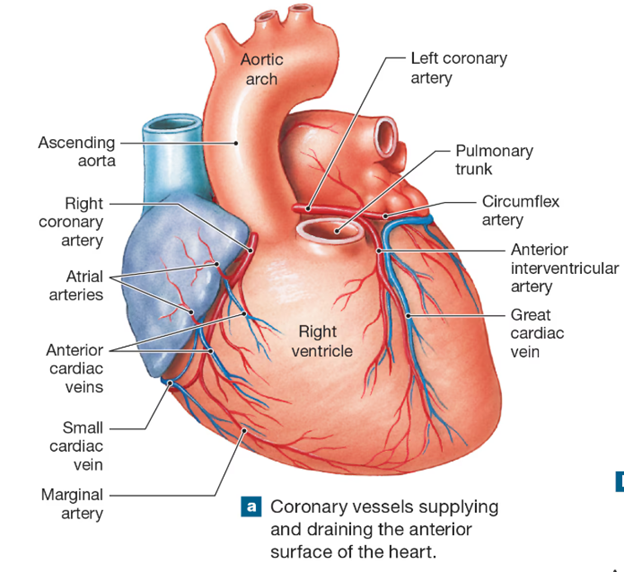
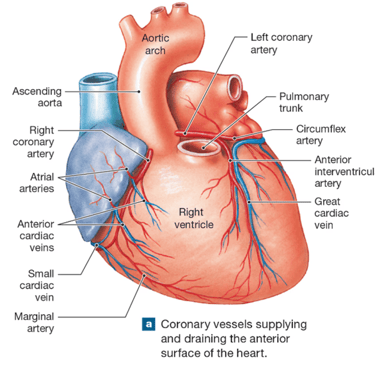
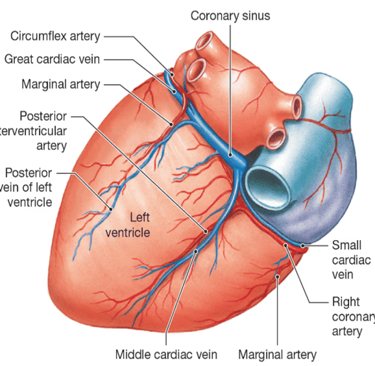
The Right Coronary Artery (RCA):
The right coronary artery originates directly from the aorta and supplies blood to the right atrium, the right ventricle, and a part of the posterior left ventricle. In around 55-60% of the population, the right coronary artery also supplies blood to the SA node (cells that are responsible for making the heart's electrical signals, making it beat). In around 85% of the population, the RCA gives rise to the posterior descending artery, supplying more blood to the right side of the heart.
The Left Coronary Artery (LCA):
The LCA splits into the left anterior descending artery (LAD) and the circumflex artery (CX). The LAD supplies blood to the front part of the interventricular septum (the division between the two ventricles), the front walls of both ventricles, and the apex of the heart (the tip of the left ventricle). The CX wraps around the left side of the heart, supplying the left atrium and the posterior part of the left ventricle.
The Coronary Sinus:
The coronary sinus is a large venous structure that collects deoxygenated blood from the heart and drains it into the right atrium. It is located in the posterior part of the heart, underneath the aortic arch, between the left atrium and left ventricle. It receives blood from multiple veins, including the great cardiac vein.
The Great Cardiac Vein:
The great cardiac vein runs alongside the LAD artery, the main vessel that pools blood into the coronary sinus. It drains blood from the anterior aspect of the heart, including the left ventricle, and empties into the coronary sinus.